Effective Alternatives to Root Canal Treatment
Introduction
Many patients – and even quite a few dentists – mistakenly believe that severe tooth pain or a deep cavity automatically requires a root canal treatment. In reality, with accurate and focused diagnostics, it’s often possible to choose more conservative approaches. Unfortunately, due to time constraints, available tools, or differing treatment philosophies, a proper targeted diagnosis is not always done, and root canal therapy becomes the default solution.
Since 2013, Dr. Sarit Avraham’s dental clinic has been a destination for people seeking a conservative, effective, and personalized solution to dental problems – even cases that in the past were considered to inevitably require a root canal. Patients from all over the country (and even abroad) turn to the clinic for a precise diagnosis and a focused treatment protocol aimed at maximally preserving the tooth’s vitality. Dr. Avraham dedicates significant time to each step of the diagnosis, and she customizes an accurate personal treatment plan for every patient.
In this article, we detail some of the alternative approaches to root canal therapy – and show how we can treat teeth deeply without compromising their vitality. In recent years, dentistry has undergone a mini-revolution with conservative, innovative approaches that allow us to preserve the tooth’s vitality even in situations once deemed irreversible. We will present two main treatment strategies:
- Vital Pulp Therapy (VPT) – treating a living pulp, even in cases of what used to be considered “irreversible” inflammation.
- Use of PRF (Platelet-Rich Fibrin) – an advanced biological approach to treat teeth with necrotic (dead) pulp.
(This article is based on broad clinical knowledge, the experience of dozens of successful treatments, and a review of over 15 up-to-date scientific papers in the field.)
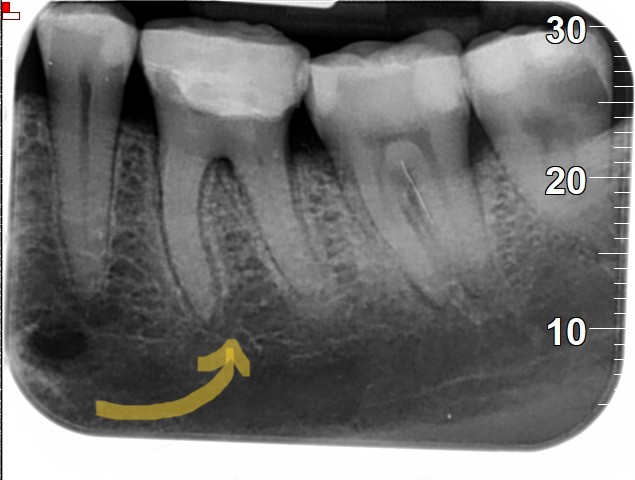
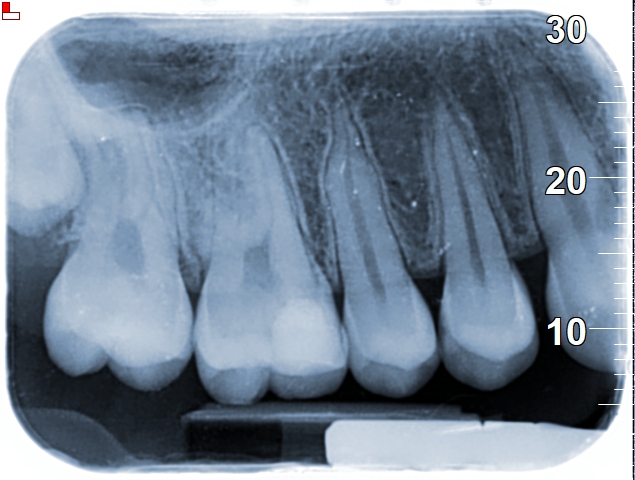
In the image below- a tooth that had a VPT instead of a Root canal treatment
Before
The patient suffered from extremely severe tooth pain, intense enough to wake her from sleep. According to conventional treatment approaches, the tooth would have required root canal therapy. A decision was made to attempt to avoid root canal treatment. Today, ten years later, this tooth is the most stable tooth in the patient’s mouth.

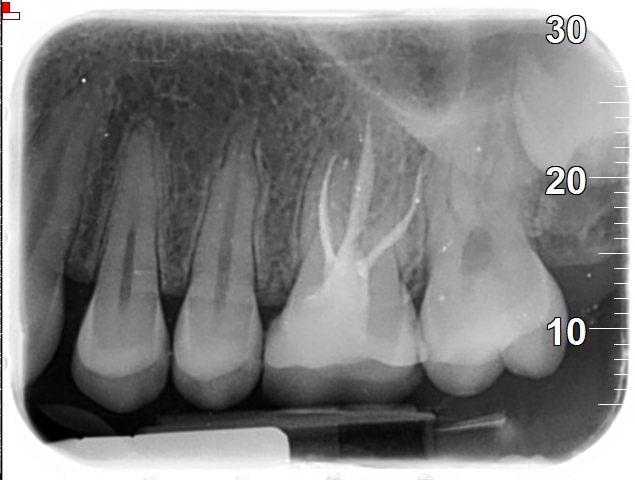
After
In the image taken ten years later, near-complete calcification of the root canals can be observed. Once the infectious factor was eliminated, a pulp capping procedure was performed (under specific conditions, as described in recent studies), and a bioactive paste promoting tertiary dentin formation was applied. The dental pulp cells were able to seal the root internally in a natural manner, without further intervention on our part, with maximal recruitment of the immune system.
What is a Root Canal Treatment?
A root canal treatment is a procedure in which the pulp tissue – the soft tissue inside the tooth – is removed due to infection or inflammation. After removing this tissue, the root canals are thoroughly cleaned and then filled and sealed with an inert material.
The pulp contains nerves and blood vessels; when it becomes irreversibly damaged or infected, the tooth can cause severe pain and may develop an abscess. A root canal is a common and effective solution to eliminate infection and pain, but it comes at a cost: it sacrifices the vitality of the tooth. In essence, a root-canal-treated tooth is no longer “alive,” as its living inner tissue has been taken out.
Limitations of Conventional Root Canals
To understand the limitations of a root canal, it’s important to know the basic structure of a tooth. Every tooth consists of two major parts:
- The outer mineralized part: The enamel is the hard, highly mineralized outer layer. Beneath it is dentin, which contains microscopic tubules and organic components (cells, collagen, fluids). These dentin tubules give the tooth slight flexibility and the ability to withstand biting forces. When a root canal is performed, the dentin tubules become exposed and tend to dry out, reducing the tooth’s flexibility and making it more brittlestoneycreekfamilydental.ca. In other words, the tooth loses some of its natural “shock absorber” quality, increasing the risk of fracture.
- The inner living part: The pulp – a soft tissue containing blood vessels, nerves, and immune cells – resides in the center (pulp chamber and root canals).
During a root canal, all of the pulp is removed – meaning we take out the living tissue that nourishes the tooth and keeps it vital from the inside. This removal weakens the tooth both biologically (no more blood supply to keep the dentin hydrated) and structurally (loss of internal tissue). Additionally, performing the root canal involves mechanical enlargement of the root canals. This step is necessary to allow thorough cleaning and proper filling, but it often requires removing a substantial amount of dentin from the canal walls. The combination of pulp removal and dentin removal can significantly reduce the tooth’s strength and resilience to fracturestoneycreekfamilydental.ca.
In recent years, scientific studies have highlighted some concerning findings about root canal outcomes:
- Approximately 23% of teeth that undergo a root canal retreatment fail within 4–5 yearspubmed.ncbi.nlm.nih.gov. In other words, nearly a quarter of retreated root canal cases do not last beyond about five years before encountering problems (persistent infection, new infection, or other failure).
- When strict evaluation criteria are used – for example, assessing healing with 3D cone-beam CT (CBCT) scans – the initial success rate of root canals can drop to around 41%pmc.ncbi.nlm.nih.gov. (By comparison, traditional 2D X-rays might overestimate success; CBCT often reveals lingering issues that 2D images miss.)
- Over the long term, the survival rate of root-canal-treated teeth declines. In one long-range observation (up to 37 years), only about 68% of root-filled teeth remained functional, meaning roughly 32% had failed in the long runpubmed.ncbi.nlm.nih.gov. In other words, about one-third of root-canal-treated teeth did not survive for the long haul (decades later they were lost or no longer functional).
Short-term issues with conventional root canals include:
- The tooth is immediately weakened by the removal of natural tissue (both pulp and some dentin). This often makes the tooth more brittle and prone to chipping or cracking if not reinforcedstoneycreekfamilydental.ca.
- There is a risk of post-treatment sensitivity or pain (for example, soreness when biting) in the days or weeks after the procedure, as the surrounding tissues recover from the intervention.
- In most cases, a crown or extensive restoration is required after a root canal to protect the tooth. Because a significant amount of tooth structure is removed, a full-coverage crown or a large onlay/inlay is typically placed to restore strength. This adds to the cost and complexity of treatment.
Long-term issues with root canals:
- A dead (non-vital) tooth is more prone to fracture. Over time, the lack of moisture and flexibility, combined with normal wear, makes root-treated teeth susceptible to cracks or catastrophic fractures.
- Significant failure rates: Newer studies indicate that more than 1 in 4 teeth that undergo a root canal will require some kind of re-intervention (retreatment, revision, or extraction) within just a few yearspubmed.ncbi.nlm.nih.govpubmed.ncbi.nlm.nih.gov. Failures can occur due to re-infection (bacteria regrowing in the canals or leaking in through an inadequate seal), fracture of the tooth, or breakdown of the root canal filling/seal.
- There is a risk of silent chronic inflammation around the root tip. Sometimes a tooth may feel fine but still harbor a smoldering infection at the root end that can go unnoticed on regular X-rays. This chronic condition can potentially affect adjacent tissues or flare up later.
- Often, a failed root canal leads to either a secondary (repeat) root canal or extraction. Retreatment of a root canal can be complex and not always successful, and if the tooth cracks or cannot be predictably fixed, extraction and replacement (with an implant or bridge) becomes the last resort.
Same patient tooth no.26
Same patient tooth no.16
The case in the image above best illustrates the importance of a more conservative approach that aims to avoid root canal treatment whenever possible. The dental radiographs shown above were taken approximately three years ago. When the patient presented to our clinic, her chief complaint was pain in tooth 26 (see radiograph above), which had previously undergone root canal treatment at another clinic. The root canal treatment on this tooth had been performed by another dentist about one year prior to her arrival to our practice.
The full story is lengthy, but in brief: a CT scan (performed in a hospital for unrelated reasons) showed that the root canal treatment in tooth 26 appeared radiographically acceptable. Typically, this tooth has four root canals, and it is quite common for the fourth canal to be missed; however, in this patient there were only three root canals, which appeared to be relatively well obturated, at least radiographically.
During the diagnostic process, the patient began to experience pain in tooth 16. A vital pulp therapy (VPT) procedure was performed, and she has remained under follow-up to this day, without any complaints of pain.
What Alternatives Exist to Root Canal?
Fortunately, modern dentistry offers alternative approaches that can avoid a full root canal in many cases. Broadly, these methods aim to treat the problem while preserving as much of the living tooth structure as possible. We will explore two primary alternatives:
Vital Pulp Therapy (VPT) – Preserving a Living Pulp
What is VPT? Vital Pulp Therapy is an umbrella term for a range of treatments designed to maintain the health and vitality of the pulp (the tooth’s inner living tissue), even when it has been exposed or inflamed. This includes certain cases that were traditionally deemed “irreversible” pulpitis, which previously would have automatically led to a root canal. In essence, instead of removing all the pulp, these therapies try to keep the healthy part of the pulp alive and only deal with the diseased portion.
Types of VPT include:
- Direct pulp capping: Placing a healing or protective material directly over an exposed pulp. (For example, if during drilling a deep cavity the pulp is pinpoint-exposed, a medicated dressing is placed on it.)
- Indirect pulp capping: When a thin layer of dentin still covers the pulp (no direct exposure), a protective biocompatible material is placed over the remaining dentin to help the pulp heal and avoid exposure.
- Partial pulpotomy: Removing a small, affected portion of the pulp (usually the inflamed part in the crown of the tooth) and leaving the rest of the pulp intact and healthy. This is sometimes called a “Cvek pulpotomy” when done after trauma, or simply partial pulp amputation of the diseased tissue.
- Full pulpotomy: Removing all the pulp tissue in the crown of the tooth (the pulp chamber), but leaving the pulp in the root canals intact and alive. The idea is to take out the irreversibly inflamed tissue in the crown, while preserving the vital pulp in the roots. The remaining pulp tissue in the canals is then treated with a biocompatible material at the canal orifices.
Why is this important? Instead of taking out all the pulp tissue and doing a full root canal, we can often remove just the damaged or infected portion of the pulp and preserve the rest. The healthy pulp that remains can then recover, heal naturally, and continue to nourish the tooth from the inside. This means the tooth stays vital (alive), which helps maintain its strength and immune defense. Over time, the preserved pulp can lay down new dentin (a process called reparative dentin formation), essentially “healing” the injury. By keeping the tooth alive, we leverage the body’s natural healing processes.
Advantages of VPT over root canal treatment:
- Preservation of vitality and natural tissue: The tooth retains its blood supply and nerve function, which keeps the dentin hydrated and resilient. The tooth essentially continues to live, potentially for many more years, instead of becoming a non-vital, brittle structure.
- Longer tooth survival: A vital tooth can respond to minor injuries and ongoing stress by remodeling and repair, which may help it last longer. By avoiding the drastic measure of a root canal, the tooth’s natural defenses remain in place, often resulting in it staying healthy and functional for many additional years.
- Reduced need for invasive procedures and extensive restorations: If we don’t do a root canal, we often don’t need to remove as much tooth structure. That can mean a smaller filling instead of a full crown, preserving more of the original tooth. This also can lower the long-term costs and complexity of dental work for the patient.
- Lower tendency to develop cracks and need extraction: Vital teeth (with intact pulp) have more inherent strength and flexibility. They are less prone to fracture compared to teeth that have undergone root canalsstoneycreekfamilydental.ca. By keeping the tooth’s internal moisture and structure, we reduce the risk that the tooth will crack and eventually need to be pulled.
- Encourages the tooth’s own healing ability: The therapies used in VPT (like calcium-enriched medicaments) encourage the pulp to heal itself by forming a dentin bridge or new hard tissue. This harnesses the tooth’s natural regenerative capacity instead of eliminating it.
When is VPT appropriate? Not every toothache or cavity can be managed with pulp therapy, but many can. General situations where VPT is considered include:
- Intense, localized pain that is indicative of pulpitis (inflammation of the pulp) but is still reversible or partially reversible. For example, a tooth with a very deep cavity causing sharp pain, but the pain is mainly with stimuli and the pulp hasn’t died yet. If the inflammation hasn’t spread beyond the pulp or caused necrosis, VPT can be an option.
- A tooth that still gives a positive response to cold tests or other vitality tests, indicating that at least part of the pulp is still alive. Even if the pain is severe, as long as some pulp tissue is living and not infected throughout, there’s a chance to save it.
- An X-ray that looks normal or shows only a small periapical change. If the radiograph is either clear or has only a very slight lesion at the root tip, it suggests the pulp may not be completely necrotic. A large abscess or spreading infection on X-ray would contraindicate VPT. In other words, VPT is suitable when we catch the problem early – before it progresses to a full-blown abscess or pulp death.
Pulp Capping: Early, Targeted Preservation
One of the most straightforward forms of VPT is pulp capping, which can often prevent a bigger issue if done promptly. When the pulp is exposed – whether due to an accident, deep decay, or during a dental treatment – it’s possible in many cases to cover it immediately and prevent inflammation from progressing.
- Direct pulp capping: used when the pulp is directly exposed (for example, during the removal of deep decay, a pin-point exposure of the pulp occurs, or after a trauma that leaves a small exposure). A biocompatible medicated material is placed right over the exposure.
- Indirect pulp capping: used when the decay is very deep but a thin layer of dentin still covers the pulp. In such cases, a dentist may choose to stop removing decay when very close to the pulp to avoid exposure. A special protective layer is then placed over the thin remaining dentin. This layer neutralizes any remaining bacteria and helps the dentin/pulp complex recover.
Typical procedure for a pulp cap:
- Gentle cleaning of the area: The dentist will carefully clean out the decayed tissue or debris, being cautious near the pulp to avoid further trauma. In indirect capping, a small amount of softened dentin might be left in place over the pulp to avoid exposure, but it is treated with disinfectants.
- Placement of a bioactive healing material: A biocompatible, calcium-rich material (commonly a product like calcium hydroxide paste or newer materials like Biodentine or MTA) is placed either directly on the exposed pulp (direct cap) or on the thin dentin layer (indirect cap). These materials stimulate the pulp to form new dentin (a dentin bridge) and have antimicrobial properties. They essentially create a seal and a healing environment for the pulp.
- Sealing and restoration: A temporary or permanent filling is then placed over the area. Often a temporary restoration is used initially to allow the pulp to heal, and after a certain period (weeks to months), the tooth is re-evaluated. If all is well (no symptoms, perhaps a follow-up X-ray looks good), a permanent filling or crown is then placed to restore the tooth’s full function and seal it long-term.
By performing a pulp cap in a timely and precise manner, the progression of inflammation can be halted and the pulp can remain alive. This early intervention is a key part of conservative dentistry – it addresses the problem at its root (literally) before it escalates into an irreversible state.
PRF Treatment for Teeth with Necrotic Pulp (Regenerative Endodontics)
What about cases where the pulp is already dead (necrotic) or the infection has advanced too far? Traditionally, the only answer was a standard root canal or extraction. However, there is now a novel biological alternative for certain cases of necrotic pulp, especially in younger patients or in specific scenarios. This approach uses the body’s own healing factors to regenerate pulp tissue. One of the most promising tools in this arena is PRF therapy.
What is PRF? PRF stands for Platelet-Rich Fibrin. It is a concentrate of the patient’s own blood components – specifically a fibrin clot that is very rich in platelets, growth factors, and healing proteins. To obtain PRF, a small sample of the patient’s blood is drawn (just like a routine blood test from the arm). This sample is then immediately spun in a centrifuge using a special protocol. The centrifugation separates the blood into layers and results in a gel-like clot of fibrin that captures a high concentration of platelets and leukocytes (white blood cells). This PRF clot is essentially a biological scaffold loaded with growth factors that can accelerate healing and tissue regeneration. Because it comes from the patient’s own blood with no additives, it’s 100% natural and biocompatible. PRF has gained widespread use in many areas of medicine and dentistry – for example, to help heal bone grafts, gum surgeries, and difficult wounds – wherever we want to encourage the body’s natural healing processes.
Using PRF in lieu of a traditional root canal: In certain cases (especially in young patients with open apexes, or even some mature teeth under careful protocols), instead of filling the cleaned canals with gutta-percha (the standard root canal filling material), the canals can be filled with a PRF clot to stimulate regeneration of the pulp tissue. The general concept and steps are:
- Careful cleaning and disinfection of the canals: Just like a root canal, the necrotic tissue and bacteria are removed from the canals. This is done gently to avoid damaging stem cells in the area. The canals are disinfected with antimicrobial solutions, but minimal or no aggressive filing is done beyond what’s necessary (to preserve stem cells in the apical area).
- Placement of PRF into the canals: The PRF membrane or pieces of the PRF clot are packed into the now-empty root canal system under sterile conditions. This is done with a precise technique, often creating a matrix in the canal. PRF acts as a biological scaffold within the canal – it fills the space and slowly releases growth factors.
- Sealing the tooth: A biocompatible material (like MTA or Biodentine) is placed over the PRF in the access opening to seal the root canal orifices, and then the tooth is restored on top (typically with a permanent filling or a crown). Over time, the presence of PRF is intended to encourage the body to regrow tissue inside the canals – essentially a process of revascularization or revitalization of the tooth.
The presence of PRF in the canal encourages the ingrowth of new blood vessels and the migration of the body’s own stem cells to form new pulp-like tissue. In regenerative endodontics, this process is sometimes called revascularization or revitalization of the tooth. The ultimate goal is for the canal to no longer be an inert, empty space but rather filled with the patient’s own vital tissue (which can potentially continue normal development of the tooth or simply reinforce the tooth from inside). Studies have found that using a PRF scaffold can lead to successful revascularization, with evidence of new tissue formation and even continued root development or thickening of canal walls in immature teethsemanticscholar.org. Essentially, we’re trying to “bioengineer” the tooth to heal itself, instead of just amputating the pulp and filling the space with artificial material.
Advantages of PRF-based regenerative treatment:
- It’s a very natural treatment – using the patient’s own blood components without any synthetic additives. This appeals to those who prefer biologically oriented therapy and reduces the chances of any adverse reaction (since it’s autologous, meaning from the patient themself).
- The tooth’s structure is preserved without the traditional root canal filling. No gutta-percha or synthetic sealers are used inside the canal in these cases, which means if the treatment is successful, the tooth has essentially a living fill (new tissue) rather than an inert one. Even if not fully “normal,” the regenerated tissue can provide some nourishment and strength to the tooth.
- PRF in the canal may help the immune system fight residual infection. The high concentration of leukocytes and growth factors in PRF could aid in eliminating any remaining bacteria and fostering an environment that is hostile to microbes. This might reduce the chance of resistant bacteria surviving and causing a repeat infection.
- This approach is applicable to both young teeth and mature teeth (with the right case selection and technique). Initially, regenerative endodontics was used primarily for young patients with developing teeth (open apices), but newer protocols and use of PRF have expanded its use to fully formed teeth in some cases.
- It avoids some complications of standard root canals. For instance, there’s no risk of leaving behind filling voids or causing certain kinds of damage from over-instrumentation, since the method relies more on biological processes. Additionally, if it works, the tooth continues to develop (in a young patient) and can achieve a better long-term prognosis than a tooth that had its growth cut short by a traditional root canal.
It should be noted that PRF treatment in necrotic teeth is part of the broader field of regenerative endodontic procedures (REPs), which are still evolving. Not every dead-tooth scenario is suitable, and success is not guaranteed (if regeneration fails, a conventional root canal might still be needed). However, the results so far are very promising, and in many cases, a previously “hopeless” tooth (by old standards) can be given a new lease on life with these advanced biological techniquessemanticscholar.org.
Conclusion: A Tooth- and Patient-Centered Approach
Root canal treatment is an important and often necessary solution – but it is not always the only option. When there is a possibility to preserve the tooth’s vitality using biological, conservative means, choosing approaches like VPT or PRF is not just about being conservative; it is advanced, safe, and human-centered. These methods aim to treat the problem while keeping the tooth as natural and alive as possible, which is better for the tooth and often better for the patient’s overall well-being.
At Dr. Sarit Avraham’s clinic, such methods are implemented with great success, thanks to precise diagnostics, rich experience, and close clinical follow-up. The philosophy is to consider both the tooth and the person – meaning the treatment is tailored to preserve natural tissues and prevent unnecessary procedures, all while ensuring the patient’s comfort and long-term health. If you have been diagnosed with pulp inflammation or are suffering from a toothache that someone said needs a root canal, it’s worth knowing that there may be another way – a more conservative, natural approach that could save your tooth’s vitality. In the era of modern dentistry, “drill and fill” is no longer the only mantra; sometimes, the best dentistry is the one that maximizes what you keep, not what you remove.
Sources: This article was informed by clinical experience and numerous scientific publications, including success rates of vital pulp therapy and regenerative endodonticspubmed.ncbi.nlm.nih.govpmc.ncbi.nlm.nih.govpubmed.ncbi.nlm.nih.gov, as well as the latest guidelines by endodontic organizations.
Recommended articles:
Regenerative approach to regain pulp vitality in mature permanent teeth using PRF vs CGF – BDJ Open, 2025
Philip N & Suneja B, Br Dent J. 2022
Lin LM et al., Aust Endod J. 2020
Chailertvanitkul P et al., Int Dent J. 2021
Keswani D et al., J Conserv Dent. 2020
Almutairi W et al., Int J Health Sci (Qassim). 2022
Goyal L et al., J Conserv Dent. 2023
Bezgin T et al., J Endod. 2015
Hilton TJ, J Am Dent Assoc. 2009
Shivashankar VY et al., J Conserv Dent. 2012
Asgary S et al., Clin Oral Investig. 2014
Taha NA et al., Int Endod J. 2017
Jadhav GR et al., J Int Soc Prev Community Dent. 2015
Aguilar P & Linsuwanont P, J Endod. 2011
Qudeimat MA et al., Int Endod J. 2017
Elmsmari F et al., Eur Arch Paediatr Dent. 2019